What is Vitreous Haemorrhage (VH)?
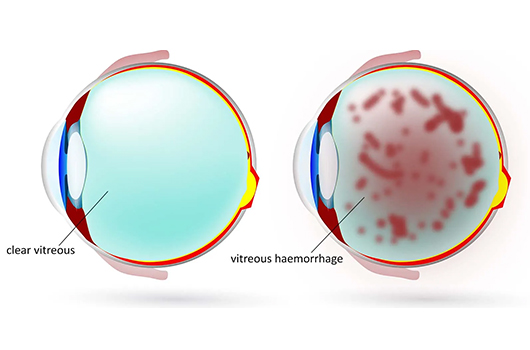
Vitreous Haemorrhage (VH) is a medical condition involving bleeding into the vitreous humor, the gel-like substance within the eye. It often stems from conditions like diabetic retinopathy, retinal tears, or age-related macular degeneration.
VH can cause sudden vision impairment characterized by floaters, dark spots, or a cloudy visual field. Prompt diagnosis and treatment are essential to address the underlying cause and potentially restore vision.
Treatment approaches range from observation and medication to surgical procedures, depending on the severity and origin of the Haemorrhage. Regular eye check-ups are crucial to monitor and manage potential risk factors for VH.