What is Diabetic Retinopathy?
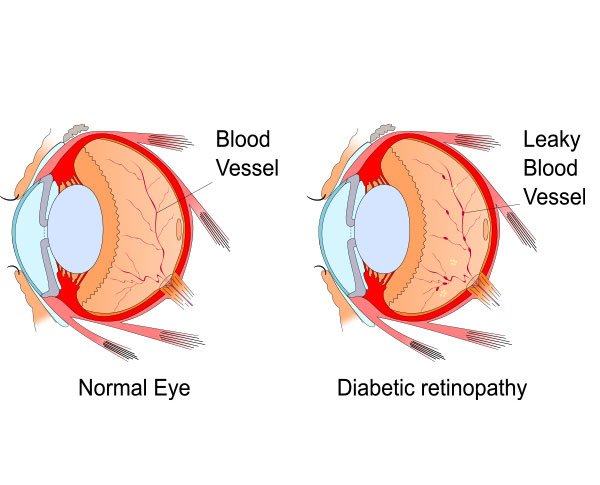
Diabetes can cause diabetic retinopathy, an eye condition that can impair vision and even blindness. Blood vessels in the retina are affected (the light-sensitive layer of tissue in the back of your eye).
If you have diabetes, it's critical to get a comprehensive dilated eye exam performed at least once a year. Even while diabetic retinopathy may not at first show any symptoms, spotting it early may allow you to take preventative measures to protect your eyesight.
You can prevent or delay vision loss by controlling your diabetes by staying active, eating well, and taking your medications.